Write your awesome label here.
Temporary Webinar Pause During
Open Enrollment
Due to the demands of Open Enrollment, you may notice a temporary pause in our regular presentations and webinars normally hosted through the university.
Agents across the nation are working tirelessly to support their communities and ensure individuals receive the guidance they need during this busy season.
We will keep you updated on when webinars will resume, returning with an even more unified and enhanced training lineup once the peak period settles.
Agents across the nation are working tirelessly to support their communities and ensure individuals receive the guidance they need during this busy season.
We will keep you updated on when webinars will resume, returning with an even more unified and enhanced training lineup once the peak period settles.
Compliance & Licensing
Compliance & Licensing Key Updates (Condensed)California Pre-licensing Reform (AB 943) California is eliminating the long-standing 20-hour pre-licensing requirement for most producer licenses starting Jan 1, 2026.
Still required: 12 hours of Ethics & CA Insurance Code (including 1 hour on fraud).
Not affected: Bail agents and public adjusters must still complete 20 hours.
By mid-January 2026, the state will deactivate all old 20/32/52-hour courses.
By mid-January 2026, the state will deactivate all old 20/32/52-hour courses.
National note: Other states are watching this shift closely as a possible future model.
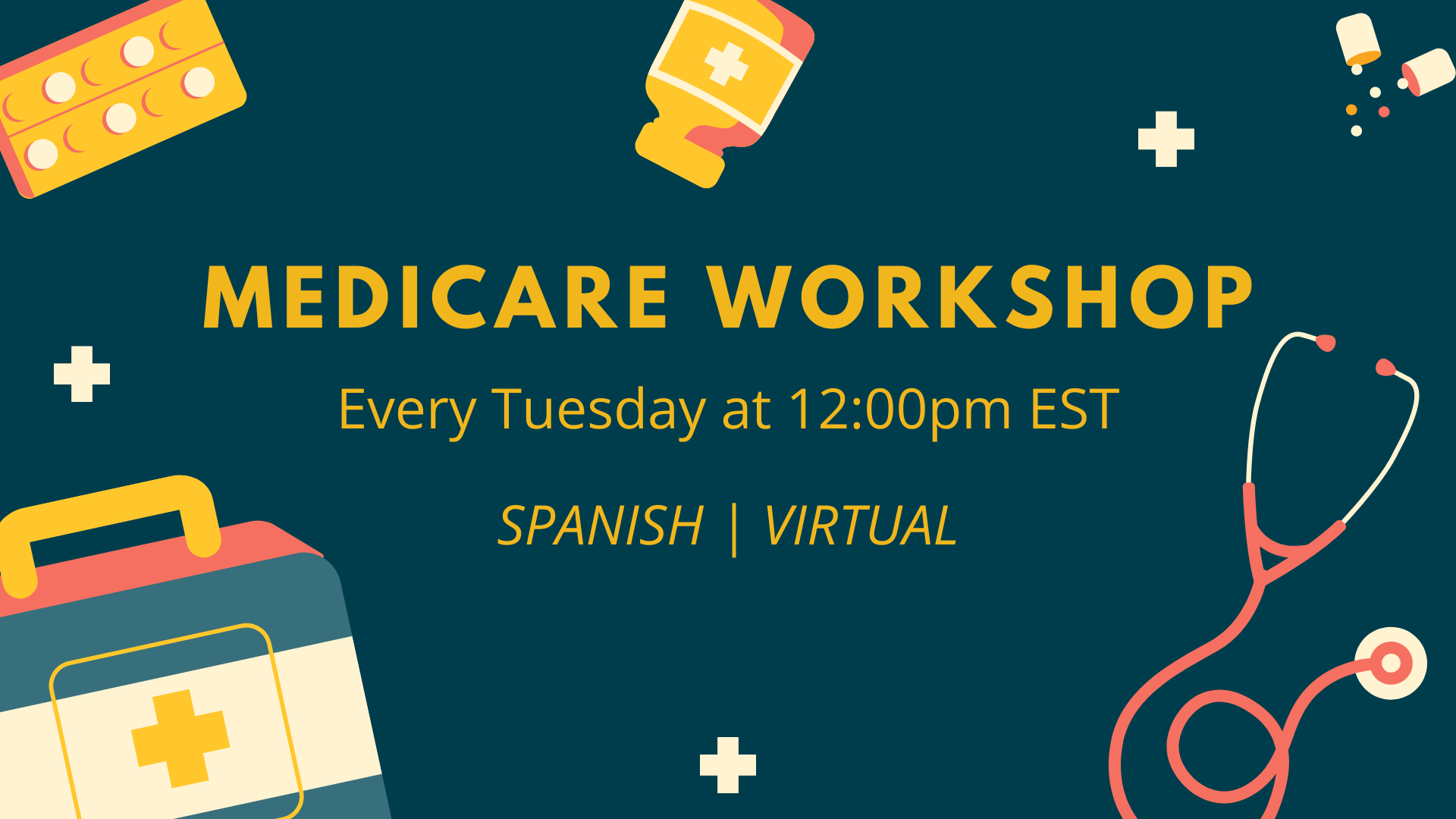
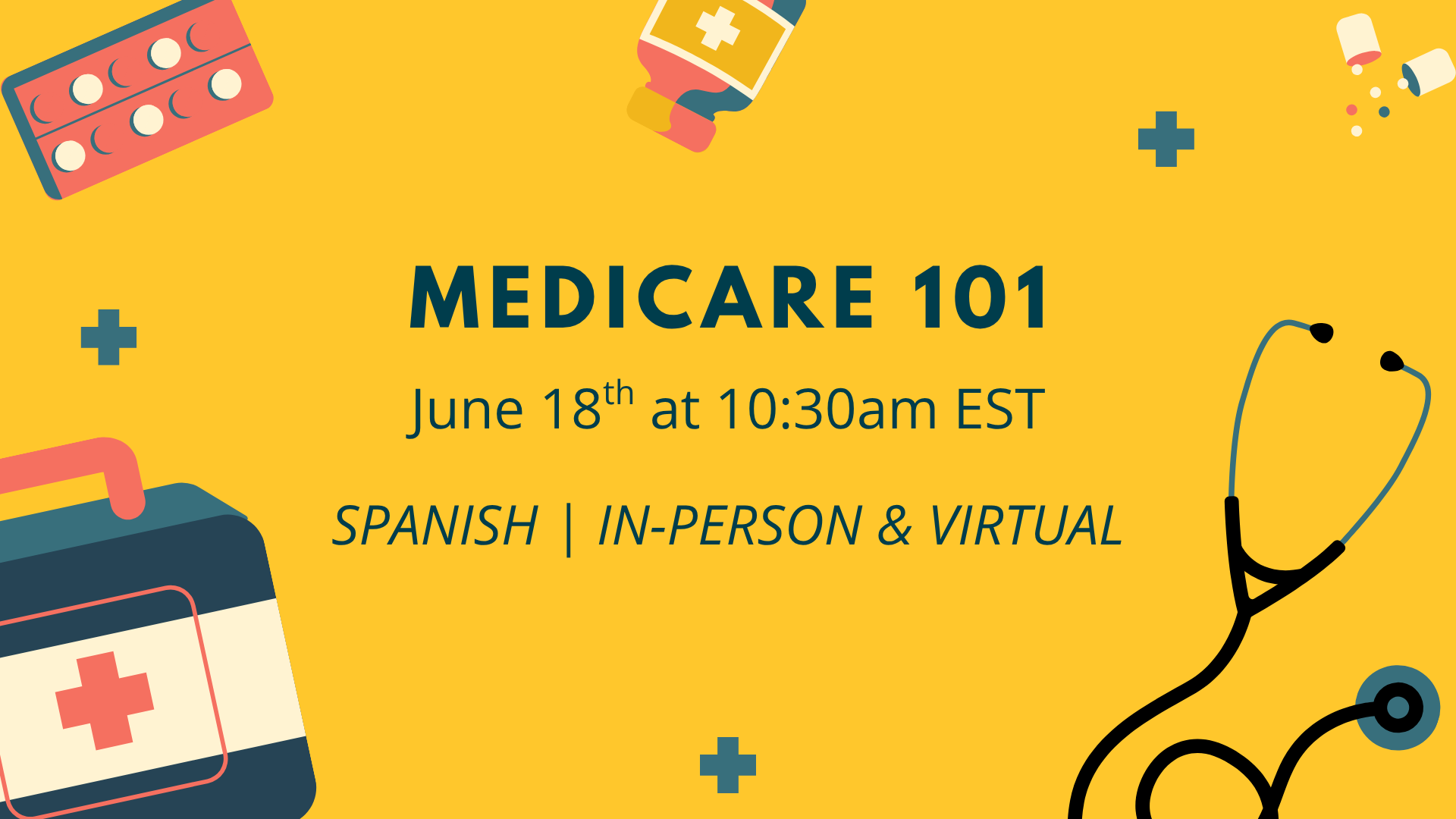
Medicare
Telehealth & 2026 Fee Schedule
What This Means for Agents
Telehealth benefits in MA remain available through at least the end of 2025.
Provider networks may shift as reimbursement changes take effect in 2026.
Brokers working with providers should expect adjustments in compensation and network participation strategies.
Telehealth Flexibility
Most pandemic-era telehealth waivers for traditional Medicare end after Sept 30, 2025, returning to rural/originating site rules.
However, Medicare Advantage plans may continue offering certain telehealth benefits through Dec 31, 2025 under temporary CMS enforcement discretion.
2026 Physician Fee Schedule (PFS) Updates
CMS’s 2026 PFS final rule includes:
Adjustments to physician payment rates. Expanded reimbursement for chronic care management, RPM/RTM, and other value-based services Continued support for behavioral health and tele-behavioral care. Updates to ACO quality measures to promote prevention and coordinated care
Marketplace (ACA)
2026 OEP & Subsidy Outlook
Open Enrollment & Binder Payments
For plan year 2026, Healthcare.gov OEP is confirmed for Nov 1 2025 - Jan 15 2026 for most states
(state-based exchanges vary)
Open Enrollment & Binder Payments
OEP for 2026 runs Nov 1, 2025 – Jan 15, 2026 for most states. For a Jan 1 start, consumers must select a plan and pay their binder—typically by Dec 31, 2025.
States like Nebraska and Pennsylvania note that members transitioning into 2026 networks must pay binder by Jan 15, 2026 to avoid gaps.
Premium Levels & Pricing Trends
CMS reports the average lowest-cost silver premium after credits will be about $50/month in 2026—$13 higher than 2025, but still lower than pre-ARP years.
Regulators emphasize: “shop, don’t auto-renew” due to changes in networks, formularies, and net premiums.
Enhanced Tax Credits with Major Uncertainty
The enhanced ACA subsidies expire at the end of 2025 unless Congress renews them. A Senate vote is expected in mid-December, but the House outlook is unclear, creating real uncertainty during Open Enrollment Period.
Analysts warn that net premiums could double for many consumers without an extension, and some regions are already seeing unusually high posted premiums because carriers priced assuming the credits end.
Marketplace 2026 Readiness
Key Points
Open Enrollment & Binder Payments
Enhanced ACA subsidies expire at the end of 2025, creating pricing uncertainty for 2026.
Premium Levels & Pricing Trends
Many carriers filed higher rates assuming subsidies will not be renewed.
Enhanced Tax Credits with Major Uncertainty
Regulators urge consumers to review networks, formularies, and cost-sharing, not just premiums.
Weekend Opening Coming Soon
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.